New Study Reveals Shared Genetic Mechanism Behind ALS, Paving the Way for Broad-Spectrum Therapies
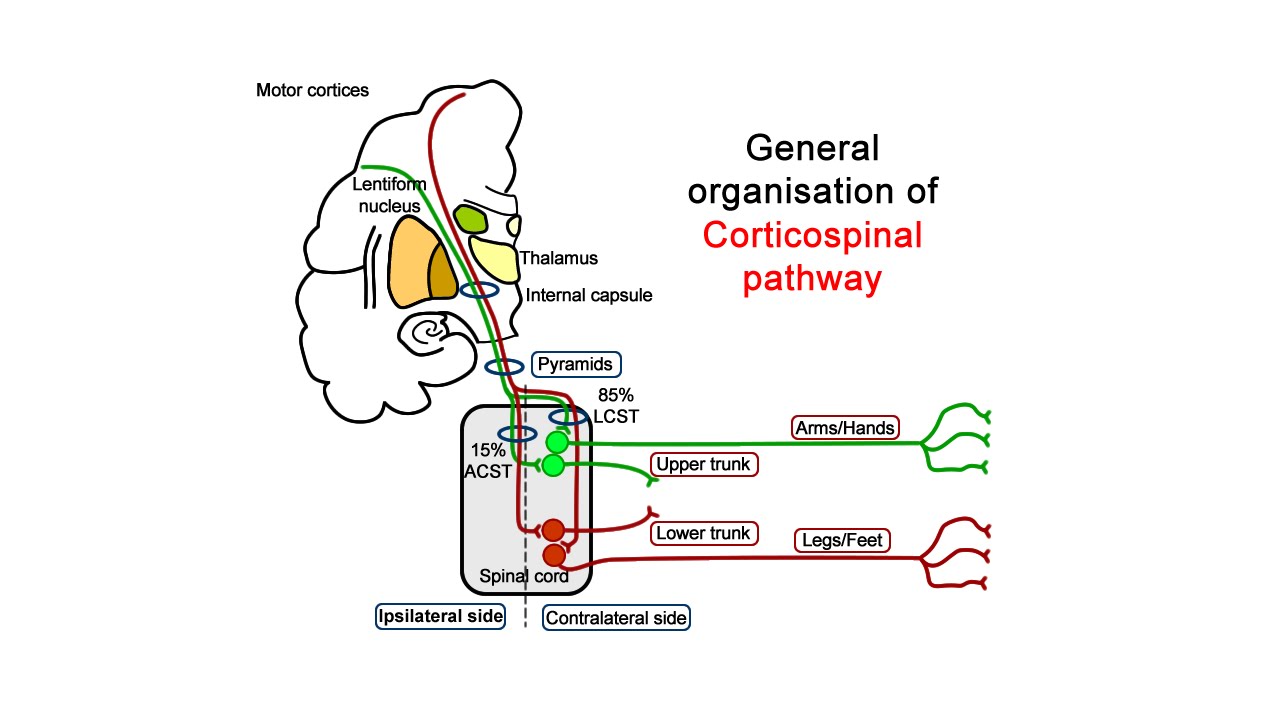
Amyotrophic lateral sclerosis (ALS)—a fatal neurodegenerative disorder known for affecting the renowned physicist Stephen Hawking—is characterized by the progressive weakening of muscles due to motor neuron degeneration. Despite numerous genetic mutations associated with ALS, developing a universal treatment has remained elusive due to the diversity in its underlying mechanisms.
Now, researchers from Tohoku University and Keio University, led by Assistant Professor Yasuaki Watanabe and Professor Keiko Nakayama, have identified a common molecular pathway that could transform how ALS is treated. Their work highlights the critical role of UNC13A, a gene essential for neuronal communication, as a potential unifying therapeutic target.
One of the hallmarks of ALS is the loss of TDP-43, a nuclear RNA-binding protein, leading to widespread RNA dysregulation. However, other RNA-binding proteins like FUS, MATR3, and hnRNPA1 are also implicated in ALS, each contributing via different pathological mechanisms. This variability has traditionally made it difficult to find shared targets for therapy.
To uncover common ground, the research team created human neural cell lines with individual knockdowns of four ALS-associated RNA-binding proteins. Remarkably, in every case, the expression of UNC13A was significantly reduced.
The team discovered two distinct mechanisms behind this downregulation:
-
Inclusion of a cryptic exon in the UNC13A transcript, leading to unstable mRNA and reduced gene expression.
-
A novel mechanism showing that loss of FUS, MATR3, or hnRNPA1 increases expression of the transcriptional repressor REST, which in turn suppresses UNC13A transcription.
Since REST acts as a silencer of gene activity, its overexpression likely contributes to the loss of UNC13A function—potentially playing a central role in ALS pathology.
To verify their findings, the researchers examined motor neurons derived from ALS patient-derived iPS cells and autopsy spinal cord tissues. In both cases, elevated levels of REST were observed, confirming the relevance of their cellular findings to actual ALS cases.
This discovery—that diverse ALS-related mutations converge on a single downstream consequence: reduced UNC13A expression—offers valuable insight into the disease’s complexity. It positions UNC13A as a central player in ALS pathogenesis and suggests that restoring its expression or inhibiting REST could serve as promising treatment strategies.
“This study provides a valuable framework for developing broad-spectrum treatments that target shared molecular vulnerabilities in ALS,” said Professor Nakayama.
As ALS advances, patients progressively lose muscle function, ultimately affecting their ability to speak, swallow, and breathe. A treatment strategy that can protect UNC13A expression in a broad range of patients could mark a significant step forward in slowing disease progression.