Immediate vs. Staged Revascularization in STEMI: Noninferiority Not Established
ESC Congress 2025 – Late-breaking research from the OPTION-STEMI trial indicates that performing immediate complete revascularization in patients with ST-segment elevation myocardial infarction (STEMI) and multivessel disease does not demonstrate noninferiority compared with a staged approach.
Background
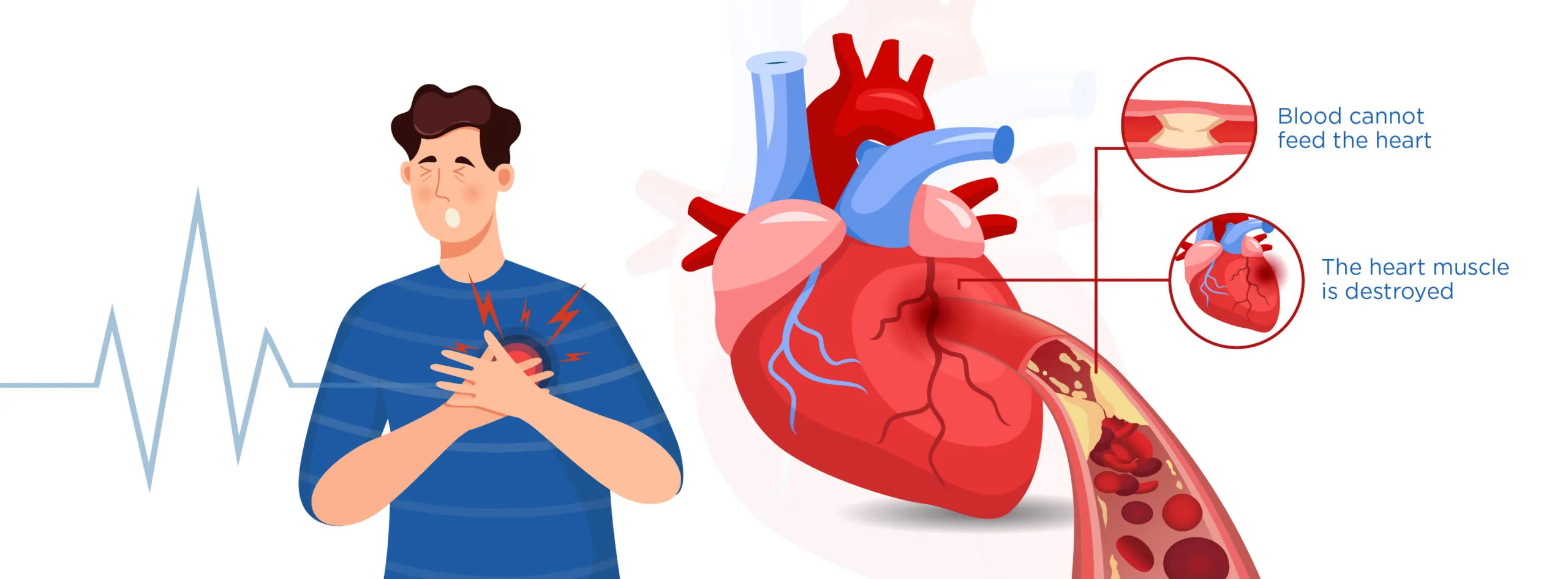
Multivessel coronary artery disease—defined as significant blockages in two or more coronary arteries—is present in nearly half of all STEMI cases. Current ESC Guidelines recommend complete revascularization using percutaneous coronary intervention (PCI), which involves treating both the culprit lesion responsible for the heart attack and the additional non-culprit lesions.
Study Objectives and Design
Professor Youngkeun Ahn (Chonnam National University Hospital, Gwangju, South Korea) and colleagues launched the OPTION-STEMI trial, an open-label, randomized study conducted at 14 South Korean centers. The trial compared two strategies:
-
Immediate complete revascularization: culprit and non-culprit lesions treated during the same PCI procedure.
-
Staged complete revascularization: culprit lesion treated first, followed by PCI for non-culprit lesions on another day during the same hospitalization.
The primary composite endpoint was all-cause death, non-fatal myocardial infarction (MI), or any unplanned revascularization at 12 months. A total of 994 patients with STEMI and multivessel disease who underwent successful culprit PCI were randomized 1:1 to either treatment arm.
Key Findings
-
Primary endpoint: occurred in 13.1% of patients undergoing immediate PCI vs. 10.8% in the staged group (HR 1.24; 95% CI 0.86–1.79; p for noninferiority=0.24), meaning noninferiority of the immediate approach was not proven.
-
Subgroup signal: Patients showing signs of heart failure (Killip class ≥II) appeared to have worse outcomes with immediate PCI (HR 1.79; 95% CI 1.05–3.05), whereas those without heart failure (Killip class I) had no excess risk (HR 0.84; 95% CI 0.50–1.41; p for interaction=0.04).
-
Secondary outcomes:
-
Non-fatal MI: 3.9% (immediate) vs. 5.1% (staged) (HR 0.77; 95% CI 0.42–1.39).
-
All-cause death: 7.5% (immediate) vs. 5.3% (staged) (HR 1.44; 95% CI 0.87–2.38).
-
-
Hospital stay: median of 4 days (immediate group) vs. 5 days (staged group); staged PCI performed ~3 days after initial procedure.
Interpretation
Professor Ahn noted:
“Immediate complete revascularization did not meet the criteria for noninferiority compared with staged revascularization. These results contrast with two recent trials that showed noninferiority for the immediate approach—but those studies either included lower-risk patients or performed staged PCI weeks later rather than during the same hospitalization.”
Clinical Implications
The findings suggest:
-
Immediate PCI may be reasonable only for stable STEMI patients with low clinical risk.
-
Patients showing signs of heart failure may benefit from a staged approach rather than immediate full revascularization.
Larger studies are warranted to confirm these findings, refine patient selection, and guide optimal timing of multivessel PCI in STEMI.