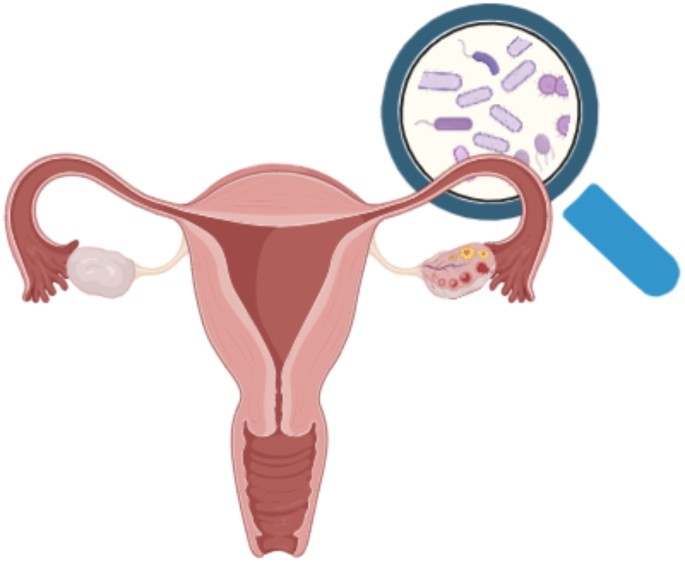
Probiotics Show Promise for Improving Ovarian Function in a Mouse Model of Premature Ovarian Insufficiency
A team of scientists from Nanjing Medical University has found that probiotics may help enhance ovarian function and modulate gut and vaginal microbiota in mice with premature ovarian insufficiency (POI) — a condition marked by an early decline in ovarian activity. Their work, published in BMC Microbiology, sheds light on the potential of microbiome-based therapies for reproductive health.
Background
Premature ovarian insufficiency, sometimes called premature menopause, affects women under the age of 40 and leads to hormonal imbalances and menstrual irregularities. Women with POI often face multiple health risks, including infertility, osteoporosis, cardiovascular disease, and cognitive issues — all of which can significantly reduce quality of life and impact mental health.
Emerging research suggests that POI may be associated with disruptions in the gut and vaginal microbiome, which could worsen hormonal imbalances and ovarian dysfunction. Building on this idea, the researchers set out to explore whether probiotics could help rebalance these microbial communities and improve ovarian health.
Study Design
In their study, the team created a POI mouse model by treating mice with cyclophosphamide, a chemotherapy drug known to damage ovarian follicles. The mice were then divided into three groups:
-
Healthy controls
-
POI mice (untreated)
-
POI mice given probiotics
The treatment group received a cocktail of 12 probiotic strains for 28 days, while the other groups were given saline. After the treatment period, the researchers measured key reproductive hormones, follicle counts, and lipid levels. They also analyzed gut and vaginal microbiota profiles from fecal and vaginal swabs.
Major Findings
Mice with induced POI showed clear signs of ovarian damage, including lower levels of anti-Müllerian hormone (AMH) and reduced numbers of developing follicles, along with increased numbers of degenerating follicles. They also had significant disruptions in their gut and vaginal microbiota compared to healthy mice.
After four weeks of probiotic supplementation, the POI mice showed trending but not statistically significant improvements in reproductive hormone levels and follicle counts. Notably, serum triglycerides dropped significantly in the treated mice, suggesting some benefit for lipid metabolism.
In terms of microbiota, probiotic treatment resulted in clear shifts in gut microbial composition, bringing it closer to that of healthy mice. Vaginal microbiota also improved, with an increased abundance of beneficial bacteria such as Rodentibacter — though the implications of this increase need further research.
Broader Implications
The findings support the idea that targeting the microbiome could help mitigate ovarian dysfunction and metabolic imbalances associated with POI. This is consistent with previous research showing that gut and vaginal microbiota play critical roles in hormonal regulation and female reproductive health.
There is evidence that gut microbes can influence vaginal immunity through circulating immune cells, while metabolites produced by gut bacteria may reach the vagina and modulate its environment.
While the results are promising, the researchers caution that these findings are preliminary and based on a mouse model. Further studies, including human clinical trials, are needed to confirm whether probiotics can effectively support ovarian function and quality of life in women with POI, particularly those affected by chemotherapy.
Looking Ahead
The team recommends future research to uncover the exact mechanisms by which probiotics influence reproductive hormones and microbiota balance. They highlight the potential of probiotics to alleviate clinical symptoms like vaginal atrophy and metabolic issues, ultimately improving long-term health for women with POI.
Clinical trials are already underway to explore this potential in human patients.